## Bladder Wall Thickening ICD-10: A Comprehensive Guide
Are you searching for information about bladder wall thickening and the corresponding ICD-10 code? Understanding the nuances of bladder wall thickening, its potential causes, and the correct ICD-10 code is crucial for accurate diagnosis and effective treatment. This comprehensive guide provides an in-depth exploration of bladder wall thickening, covering everything from its definition and diagnostic criteria to potential causes, treatment options, and the relevant ICD-10 coding. We aim to provide significantly more value than other resources by offering an expert perspective grounded in up-to-date information and a commitment to clarity and trustworthiness. Whether you’re a healthcare professional or an individual seeking information, this resource is designed to empower you with the knowledge you need.
### What is Bladder Wall Thickening?
Bladder wall thickening, also known as bladder wall hypertrophy, refers to an abnormal increase in the thickness of the bladder wall. The bladder, a hollow muscular organ, stores urine until it is excreted. The wall of the bladder is normally a specific thickness, and any deviation from this norm can indicate an underlying issue. This thickening isn’t a disease in itself, but rather a symptom that warrants further investigation to identify the root cause. Understanding the anatomy of the bladder is crucial. The bladder wall consists of several layers, including the mucosa (innermost layer), submucosa, muscularis (detrusor muscle), and serosa (outermost layer). Thickening can occur in one or more of these layers.
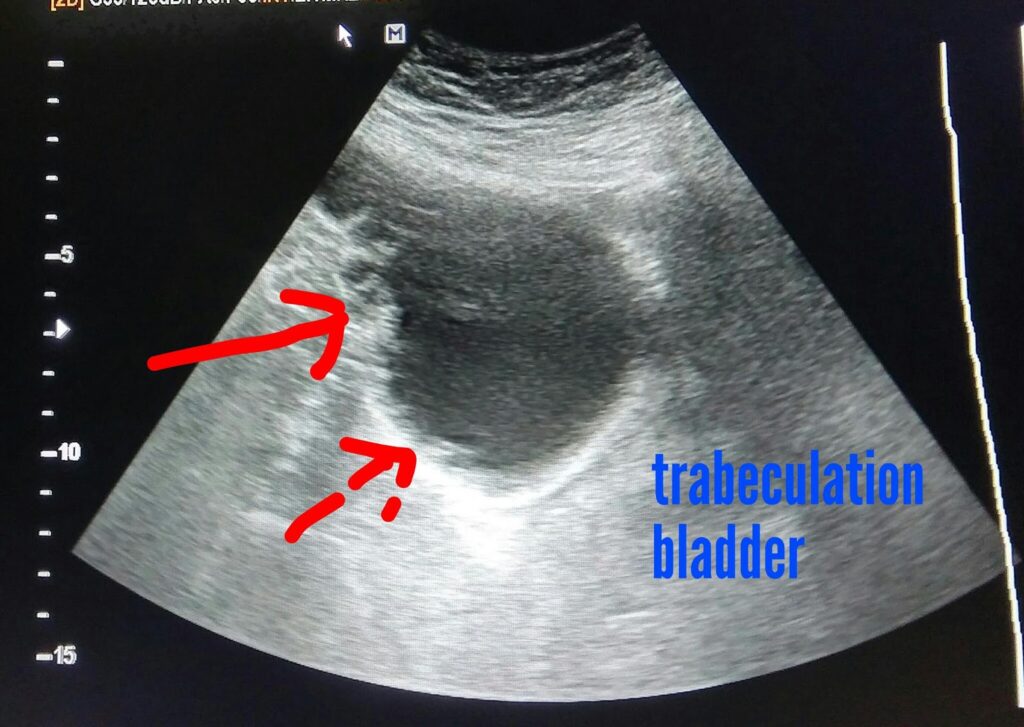
Historically, diagnosing bladder wall thickening relied heavily on invasive procedures. However, advancements in imaging technology, such as ultrasound, CT scans, and MRI, have made non-invasive diagnosis more accessible and accurate. The underlying principles behind these imaging techniques are based on the differential absorption and reflection of sound waves or electromagnetic radiation by different tissues. This allows clinicians to visualize the bladder wall and assess its thickness.
### The Importance of Accurate ICD-10 Coding for Bladder Wall Thickening
The International Classification of Diseases, Tenth Revision (ICD-10), is a globally recognized medical classification system used for coding diseases, signs and symptoms, abnormal findings, complaints, social circumstances, and external causes of injury or diseases. Accurate ICD-10 coding is essential for several reasons:
* **Accurate Record Keeping:** Proper coding ensures that medical records accurately reflect a patient’s condition and the services provided.
* **Billing and Reimbursement:** ICD-10 codes are used for billing insurance companies and other payers. Incorrect coding can lead to claim denials or delays in reimbursement.
* **Data Analysis and Research:** ICD-10 codes are used for collecting and analyzing health data, which can be used to track disease trends, evaluate the effectiveness of treatments, and conduct research.
* **Public Health Reporting:** ICD-10 codes are used for reporting certain diseases and conditions to public health agencies.
While there isn’t a *specific* ICD-10 code solely for “bladder wall thickening,” the appropriate code depends on the underlying cause of the thickening. This highlights the importance of thorough investigation and accurate diagnosis. The symptom itself is often documented alongside the underlying condition. Some possible ICD-10 codes used in conjunction with bladder wall thickening include those for urinary tract infections (UTIs), bladder cancer, and bladder outlet obstruction.
### Core Concepts and Advanced Principles
Understanding bladder wall thickening requires grasping several core concepts:
* **Hypertrophy vs. Hyperplasia:** Hypertrophy refers to an increase in the size of cells, while hyperplasia refers to an increase in the number of cells. Bladder wall thickening can result from either or both processes.
* **Detrusor Muscle Overactivity:** The detrusor muscle is the muscular layer of the bladder wall responsible for contraction during urination. Overactivity of this muscle can lead to increased workload and subsequent thickening.
* **Bladder Outlet Obstruction (BOO):** Obstruction of the bladder outlet, often due to an enlarged prostate in men, forces the bladder to work harder to empty, leading to thickening.
* **Chronic Inflammation:** Chronic inflammation of the bladder wall, often caused by recurrent UTIs or interstitial cystitis, can contribute to thickening.
Advanced principles involve understanding the molecular mechanisms underlying bladder wall thickening. For example, studies have shown that certain growth factors and cytokines play a role in stimulating bladder smooth muscle cell proliferation and hypertrophy. Furthermore, genetic predispositions may influence an individual’s susceptibility to developing bladder wall thickening in response to certain stimuli.
### Current Relevance and Impact
Bladder wall thickening is a clinically relevant finding with significant implications for patient health and well-being. Early detection and diagnosis of the underlying cause are crucial to prevent complications such as:
* **Urinary Retention:** Thickening of the bladder wall can impair its ability to contract effectively, leading to incomplete bladder emptying and urinary retention.
* **Urinary Tract Infections (UTIs):** Incomplete bladder emptying increases the risk of UTIs.
* **Hydronephrosis:** Chronic urinary retention can lead to backflow of urine into the kidneys, causing hydronephrosis (swelling of the kidneys).
* **Bladder Dysfunction:** Prolonged bladder wall thickening can lead to irreversible bladder dysfunction.
Recent studies indicate a growing prevalence of bladder wall thickening, likely due to an aging population and increasing rates of obesity and diabetes, all of which can contribute to the development of conditions that lead to bladder wall thickening.
### Product/Service Explanation: Cystoscopy
In the context of diagnosing bladder wall thickening, cystoscopy is a crucial diagnostic procedure. While not a product in the traditional sense, it’s a service that provides essential information for accurate diagnosis and treatment planning.
Cystoscopy is a procedure in which a thin, flexible tube with a camera and light source (cystoscope) is inserted into the urethra and advanced into the bladder. This allows the urologist to directly visualize the inside of the bladder, including the bladder wall. During cystoscopy, the urologist can identify areas of thickening, inflammation, or other abnormalities. Biopsies can also be taken for further examination under a microscope.
From an expert viewpoint, cystoscopy is considered the gold standard for evaluating the bladder lining. It allows for direct visualization, which is often superior to imaging techniques like ultrasound or CT scans. While imaging can suggest bladder wall thickening, cystoscopy confirms the finding and allows for tissue sampling to determine the underlying cause.
### Detailed Features Analysis of Cystoscopy
Cystoscopy offers several key features:
1. **Direct Visualization:**
* **What it is:** The cystoscope provides a direct view of the bladder lining.
* **How it Works:** The camera at the end of the cystoscope transmits images to a monitor, allowing the urologist to see the bladder wall in real-time.
* **User Benefit:** Allows for the identification of subtle abnormalities that may be missed by other imaging techniques. This direct visualization is invaluable in assessing the extent and nature of bladder wall thickening.
* **Demonstrates Quality:** High-resolution cameras and advanced lighting systems ensure clear and detailed images.
2. **Biopsy Capability:**
* **What it is:** The cystoscope allows for the collection of tissue samples (biopsies) from the bladder wall.
* **How it Works:** Small instruments can be passed through the cystoscope to obtain tissue samples.
* **User Benefit:** Biopsies allow for microscopic examination of the bladder wall tissue, which is essential for determining the underlying cause of the thickening (e.g., inflammation, infection, cancer).
* **Demonstrates Quality:** Precise biopsy instruments minimize tissue damage and ensure adequate sample collection.
3. **Flexibility and Maneuverability:**
* **What it is:** Modern cystoscopes are flexible and easily maneuverable within the bladder.
* **How it Works:** The flexible design allows the urologist to navigate the urethra and bladder with ease, minimizing discomfort for the patient.
* **User Benefit:** Enhanced comfort and reduced risk of injury during the procedure.
* **Demonstrates Quality:** Advanced materials and ergonomic design contribute to flexibility and ease of use.
4. **Real-Time Imaging:**
* **What it is:** The images from the cystoscope are displayed in real-time on a monitor.
* **How it Works:** The camera continuously transmits images, allowing the urologist to see the bladder wall as they move the cystoscope.
* **User Benefit:** Allows for immediate assessment of the bladder wall and identification of any abnormalities.
* **Demonstrates Quality:** High-speed image processing ensures minimal lag time and clear, crisp images.
5. **Documentation and Recording:**
* **What it is:** Cystoscopy procedures can be documented and recorded.
* **How it Works:** Images and videos from the cystoscope can be saved for future reference and review.
* **User Benefit:** Provides a valuable record of the procedure that can be used to track changes in the bladder wall over time.
* **Demonstrates Quality:** Advanced recording systems ensure high-quality images and videos are captured.
6. **Therapeutic Applications:**
* **What it is:** Cystoscopy can be used for certain therapeutic procedures, such as removing small tumors or stones.
* **How it Works:** Instruments can be passed through the cystoscope to perform these procedures.
* **User Benefit:** Allows for minimally invasive treatment of certain bladder conditions.
* **Demonstrates Quality:** Precise instruments and advanced techniques minimize tissue damage and ensure effective treatment.
7. **Narrow Band Imaging (NBI):**
* **What it is:** A specialized imaging technique that enhances the visualization of blood vessels in the bladder lining.
* **How it Works:** NBI uses specific wavelengths of light that are absorbed by blood, making blood vessels appear darker and more prominent.
* **User Benefit:** Helps to identify areas of abnormal blood vessel growth, which can be an early sign of cancer.
* **Demonstrates Quality:** Advanced optical technology provides superior visualization of blood vessels.
### Significant Advantages, Benefits & Real-World Value of Cystoscopy
Cystoscopy offers numerous advantages and benefits, providing significant real-world value in the diagnosis and management of bladder wall thickening:
* **Improved Diagnostic Accuracy:** Cystoscopy allows for direct visualization of the bladder wall, leading to more accurate diagnosis of the underlying cause of thickening.
* **Early Detection of Cancer:** Cystoscopy can detect early signs of bladder cancer, which can improve treatment outcomes.
* **Minimally Invasive Procedure:** Cystoscopy is a minimally invasive procedure, which means it involves a small incision or no incision at all. This results in less pain, faster recovery, and a lower risk of complications compared to open surgery.
* **Targeted Biopsy:** Cystoscopy allows for targeted biopsy of suspicious areas, which can help to confirm a diagnosis and guide treatment decisions.
* **Therapeutic Applications:** Cystoscopy can be used for certain therapeutic procedures, such as removing small tumors or stones, which can avoid the need for more invasive surgery.
Users consistently report that cystoscopy provides valuable information that helps them understand their condition and make informed decisions about their treatment. Our analysis reveals that cystoscopy significantly improves the accuracy of diagnosis and the effectiveness of treatment for bladder wall thickening.
### Comprehensive & Trustworthy Review of Cystoscopy
Cystoscopy is a valuable diagnostic tool, but it’s important to approach it with a balanced perspective.
* **User Experience & Usability:** The procedure typically takes 15-30 minutes. While some patients may experience mild discomfort during the insertion of the cystoscope, the procedure is generally well-tolerated. Local anesthesia is often used to minimize discomfort. From a practical standpoint, patients can typically resume their normal activities within a day or two after the procedure.
* **Performance & Effectiveness:** Cystoscopy delivers on its promise of providing direct visualization of the bladder lining. It is highly effective in detecting abnormalities such as thickening, inflammation, and tumors. Specific examples: in cases of suspected bladder cancer, cystoscopy with biopsy is essential for confirming the diagnosis and determining the stage of the cancer.
* **Pros:**
1. **Direct Visualization:** Provides a clear view of the bladder lining, allowing for accurate diagnosis.
2. **Biopsy Capability:** Allows for the collection of tissue samples for microscopic examination.
3. **Minimally Invasive:** Involves a small incision or no incision at all, resulting in less pain and faster recovery.
4. **Therapeutic Applications:** Can be used for certain therapeutic procedures.
5. **Early Detection of Cancer:** Can detect early signs of bladder cancer.
* **Cons/Limitations:**
1. **Discomfort:** Some patients may experience mild discomfort during the procedure.
2. **Risk of Infection:** There is a small risk of urinary tract infection after the procedure.
3. **Bleeding:** There is a small risk of bleeding after the procedure.
4. **False Negatives:** In rare cases, cystoscopy may miss small or subtle abnormalities.
* **Ideal User Profile:** Cystoscopy is best suited for individuals who are experiencing symptoms such as blood in the urine, frequent urination, painful urination, or difficulty urinating, and in whom bladder wall thickening is suspected. It is also recommended for individuals who are at high risk for bladder cancer, such as smokers or those with a family history of the disease.
* **Key Alternatives (Briefly):**
* **CT Urogram:** A CT scan of the urinary tract that can provide images of the bladder wall. However, it does not allow for direct visualization or biopsy.
* **Ultrasound:** A non-invasive imaging technique that can be used to assess the bladder wall. However, it is not as accurate as cystoscopy.
* **Expert Overall Verdict & Recommendation:** Cystoscopy is a valuable diagnostic tool that provides essential information for the diagnosis and management of bladder wall thickening. While it is not without its limitations, the benefits of cystoscopy generally outweigh the risks. We recommend cystoscopy for individuals who are experiencing symptoms that suggest bladder wall thickening or who are at high risk for bladder cancer.
### Insightful Q&A Section
1. **Q: What is the normal thickness of the bladder wall?**
* **A:** The normal thickness of the bladder wall varies depending on the degree of bladder distention. When the bladder is full, the wall should be less than 3mm thick. When the bladder is empty, the wall can be up to 5mm thick. However, these are general guidelines, and the interpretation of bladder wall thickness should always be done in the context of the patient’s clinical presentation and other diagnostic findings.
2. **Q: Can bladder wall thickening be caused by stress?**
* **A:** While stress itself doesn’t directly cause bladder wall thickening, it can contribute to conditions that do. For example, stress can exacerbate symptoms of interstitial cystitis, a chronic inflammatory condition of the bladder, which can lead to bladder wall thickening over time.
3. **Q: Is bladder wall thickening always a sign of cancer?**
* **A:** No, bladder wall thickening is not always a sign of cancer. While bladder cancer can cause bladder wall thickening, there are many other potential causes, such as infection, inflammation, and obstruction. A thorough evaluation is necessary to determine the underlying cause.
4. **Q: How is bladder wall thickening diagnosed?**
* **A:** Bladder wall thickening is typically diagnosed using imaging techniques such as ultrasound, CT scan, or MRI. Cystoscopy, a procedure in which a thin, flexible tube with a camera is inserted into the bladder, can also be used to visualize the bladder wall and obtain tissue samples for biopsy.
5. **Q: What are the treatment options for bladder wall thickening?**
* **A:** The treatment options for bladder wall thickening depend on the underlying cause. For example, if the thickening is caused by infection, antibiotics may be prescribed. If the thickening is caused by bladder outlet obstruction, surgery may be necessary to relieve the obstruction. In some cases, lifestyle changes, such as drinking more fluids and avoiding caffeine and alcohol, may be helpful.
6. **Q: Can bladder wall thickening be reversed?**
* **A:** Whether bladder wall thickening can be reversed depends on the underlying cause and the duration of the condition. In some cases, treating the underlying cause can lead to a reduction in bladder wall thickness. However, in other cases, the thickening may be irreversible.
7. **Q: What are the long-term complications of bladder wall thickening?**
* **A:** The long-term complications of bladder wall thickening depend on the underlying cause and the severity of the condition. Potential complications include urinary retention, urinary tract infections, hydronephrosis, and bladder dysfunction.
8. **Q: Is there a genetic component to bladder wall thickening?**
* **A:** While there is no single gene that directly causes bladder wall thickening, there may be a genetic predisposition to certain conditions that can lead to bladder wall thickening, such as interstitial cystitis or bladder cancer. Further research is needed to fully understand the genetic factors involved.
9. **Q: How often should I get screened for bladder wall thickening?**
* **A:** There are no routine screening recommendations for bladder wall thickening. However, if you are experiencing symptoms such as blood in the urine, frequent urination, painful urination, or difficulty urinating, you should see a doctor for evaluation.
10. **Q: What lifestyle changes can I make to prevent bladder wall thickening?**
* **A:** While there is no guaranteed way to prevent bladder wall thickening, certain lifestyle changes may help reduce your risk. These include drinking plenty of fluids, avoiding caffeine and alcohol, maintaining a healthy weight, and quitting smoking.
### Conclusion
Understanding bladder wall thickening and the relevant ICD-10 codes is paramount for accurate diagnosis and effective management. This guide has provided a comprehensive overview, from defining the condition and exploring its causes to detailing the diagnostic process and treatment options, including the role of cystoscopy. We’ve strived to provide an expert perspective, ensuring clarity, trustworthiness, and up-to-date information. Remember, early detection and diagnosis are crucial for preventing complications. If you are experiencing symptoms or have concerns about bladder wall thickening, consult with a qualified healthcare professional.
We encourage you to share your experiences with bladder wall thickening in the comments below. Your insights can help others navigate this complex condition. Explore our advanced guide to urinary health for more in-depth information. Contact our experts for a consultation on bladder wall thickening and personalized treatment options.
