Food Poisoning and Breastfeeding: A Comprehensive Guide for Nursing Mothers
Experiencing food poisoning while breastfeeding can be a distressing experience. Concerns about the safety of your breast milk and the well-being of your baby are paramount. This comprehensive guide addresses these concerns head-on, providing expert advice, practical strategies, and reassurance to help you navigate this challenging situation with confidence. We aim to provide a resource that goes beyond basic information, offering in-depth insights and evidence-based recommendations to ensure both your health and your baby’s safety during this time. This guide provides everything you need to know about food poisoning and breastfeeding.
Understanding Food Poisoning and Breastfeeding
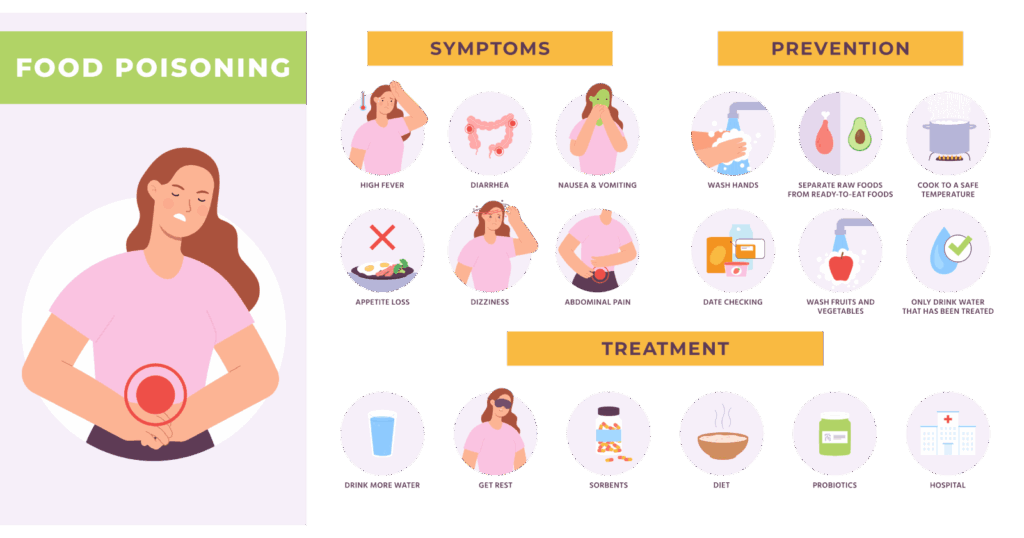
Food poisoning, also known as foodborne illness, is caused by consuming contaminated food or beverages. Bacteria, viruses, and parasites are the most common culprits. Symptoms can range from mild discomfort to severe illness, including nausea, vomiting, diarrhea, abdominal cramps, and fever. While incredibly unpleasant for anyone, it raises specific concerns for breastfeeding mothers. Can the pathogens pass through breast milk? How does it affect milk supply? These questions are central to understanding the relationship between food poisoning and breastfeeding.
What Causes Food Poisoning?
Food poisoning occurs when harmful microorganisms contaminate food at any stage of production, processing, or preparation. Common causes include:
* **Bacteria:** Salmonella, E. coli, Listeria, Campylobacter, and Staphylococcus aureus are frequent offenders.
* **Viruses:** Norovirus and rotavirus are often spread through contaminated food or water.
* **Parasites:** Giardia, Cryptosporidium, and Cyclospora can also cause foodborne illness.
Improper food handling, inadequate cooking temperatures, and poor hygiene practices contribute significantly to the spread of these contaminants.
How Common is Food Poisoning?
Food poisoning is a widespread issue. According to the Centers for Disease Control and Prevention (CDC), millions of people in the United States experience food poisoning each year. While most cases are mild and resolve on their own, some can lead to serious complications, especially for vulnerable populations like infants and pregnant or breastfeeding women.
Is Food Poisoning Transmitted Through Breast Milk?
This is the primary concern for breastfeeding mothers. Generally, the pathogens that cause food poisoning are *not* transmitted through breast milk. Your body filters most of these harmful microorganisms, preventing them from reaching your baby via breast milk. However, dehydration and fever, common symptoms of food poisoning, can indirectly affect milk supply and overall well-being.
The Importance of Staying Hydrated
Dehydration is a significant risk associated with food poisoning. Vomiting and diarrhea can quickly deplete your body’s fluids, impacting milk production. Maintaining adequate hydration is crucial for sustaining your milk supply and ensuring your baby receives sufficient nourishment. Aim to drink plenty of water, electrolyte solutions, or herbal teas. Monitoring urine color is a good indicator of hydration levels; pale yellow indicates adequate hydration, while dark yellow suggests dehydration.
Managing Food Poisoning While Breastfeeding: Expert Strategies
Managing food poisoning while breastfeeding requires a multifaceted approach that prioritizes both your recovery and your baby’s health. Here are expert strategies to consider:
1. Prioritize Hydration
As mentioned earlier, hydration is paramount. Drink small, frequent sips of clear fluids. Oral rehydration solutions (ORS) can help replenish electrolytes lost through vomiting and diarrhea. Avoid sugary drinks, as they can sometimes worsen diarrhea. Herbal teas, such as chamomile or ginger, can soothe your stomach and promote relaxation.
2. Continue Breastfeeding
Unless specifically advised otherwise by your doctor, continue breastfeeding. As stated above, the pathogens that cause food poisoning are not typically transmitted through breast milk. Breastfeeding provides your baby with essential antibodies and nutrients that can help protect them from illness. Frequent breastfeeding can also help maintain your milk supply during this time.
3. Monitor Your Baby Closely
Pay close attention to your baby’s behavior and health. Look for signs of illness, such as fever, vomiting, diarrhea, or changes in feeding patterns. If you notice any concerning symptoms, contact your pediatrician immediately. While it’s unlikely your baby will contract the food poisoning directly from your breast milk, they may be more susceptible to other illnesses if your immune system is compromised.
4. Consider Medication (With Caution)
Over-the-counter medications for diarrhea and vomiting should be used with caution while breastfeeding. Some medications may pass into breast milk and could potentially affect your baby. Always consult with your doctor or a lactation consultant before taking any medication. In some cases, prescription medications may be necessary to treat severe food poisoning. Your doctor can recommend the safest options for you and your baby.
5. Rest and Recovery
Allow your body ample time to rest and recover. Food poisoning can be physically draining. Delegate household tasks and childcare responsibilities to your partner, family members, or friends. Prioritize sleep and avoid strenuous activities. A well-rested body is better equipped to fight off infection and maintain milk supply.
6. Practice Strict Hygiene
Maintain strict hygiene practices to prevent the spread of infection. Wash your hands thoroughly with soap and water before and after breastfeeding, preparing food, or using the restroom. Disinfect surfaces that may have come into contact with vomit or diarrhea. Proper hygiene is essential for protecting both yourself and your baby.
7. Consult with Healthcare Professionals
Don’t hesitate to seek professional medical advice. Consult with your doctor, a lactation consultant, or a registered dietitian for personalized guidance. They can assess your specific situation, recommend appropriate treatment options, and provide support to help you navigate food poisoning while breastfeeding.
Food Poisoning Treatment Options Compatible with Breastfeeding
Choosing the right treatment options while breastfeeding is crucial to ensure both your safety and your baby’s well-being. Here’s a breakdown of common treatments and their compatibility with breastfeeding:
Oral Rehydration Solutions (ORS)
* **What it is:** ORS are specifically formulated to replenish fluids and electrolytes lost through vomiting and diarrhea.
* **How it works:** They contain a balanced mixture of salts and sugars that help your body absorb fluids more effectively.
* **User benefit:** Prevents dehydration, supports milk supply, and promotes faster recovery.
* **Breastfeeding compatibility:** Generally considered safe for breastfeeding mothers. Always follow the manufacturer’s instructions.
Probiotics
* **What it is:** Probiotics are live microorganisms that can help restore the balance of good bacteria in your gut.
* **How it works:** They compete with harmful bacteria, reducing inflammation and improving digestive function.
* **User benefit:** May shorten the duration of diarrhea and alleviate other symptoms of food poisoning.
* **Breastfeeding compatibility:** Many probiotics are considered safe for breastfeeding, but it’s best to consult with your doctor before starting any new supplement.
Anti-Nausea Medications
* **What it is:** Medications designed to relieve nausea and vomiting.
* **How it works:** Different types of anti-nausea medications work through various mechanisms to calm the stomach and reduce the urge to vomit.
* **User benefit:** Provides relief from nausea and vomiting, allowing you to stay hydrated and eat small, bland meals.
* **Breastfeeding compatibility:** Some anti-nausea medications are considered safer than others for breastfeeding. Discuss your options with your doctor to determine the best choice for you.
Activated Charcoal
* **What it is:** A substance that can absorb toxins and bacteria in the digestive system.
* **How it works:** It binds to harmful substances, preventing them from being absorbed into the bloodstream.
* **User benefit:** May help reduce the severity and duration of food poisoning symptoms.
* **Breastfeeding compatibility:** Limited research exists on the safety of activated charcoal during breastfeeding. Consult with your doctor before using it.
Antibiotics
* **What it is:** Medications used to treat bacterial infections.
* **How it works:** They kill or inhibit the growth of bacteria, helping your body fight off the infection.
* **User benefit:** Effective for treating severe cases of bacterial food poisoning.
* **Breastfeeding compatibility:** Some antibiotics are safe for breastfeeding, while others are not. Your doctor will prescribe an antibiotic that is compatible with breastfeeding if needed.
Advantages of Continuing Breastfeeding During Food Poisoning
Continuing to breastfeed during food poisoning offers several significant advantages for both you and your baby:
* **Provides Essential Antibodies:** Breast milk contains antibodies that can protect your baby from illness, even if you are sick. These antibodies can help boost your baby’s immune system and reduce their risk of infection.
* **Maintains Milk Supply:** Frequent breastfeeding helps maintain your milk supply, ensuring that your baby continues to receive adequate nourishment. Dehydration and stress can reduce milk production, so continuing to breastfeed regularly is crucial.
* **Offers Comfort and Security:** Breastfeeding provides comfort and security for your baby, especially when you are not feeling well. The act of nursing can help calm and soothe your baby, reducing their anxiety and promoting bonding.
* **Reduces the Risk of Allergies:** Breast milk contains substances that can help prevent allergies in your baby. Continuing to breastfeed, even when you are sick, can help protect your baby from developing allergies later in life.
* **Promotes Gut Health:** Breast milk contains prebiotics that promote the growth of beneficial bacteria in your baby’s gut. This can help improve digestion and reduce the risk of gastrointestinal problems.
* **Facilitates Recovery:** The hormones released during breastfeeding can help promote your recovery from food poisoning. These hormones can reduce stress, promote relaxation, and help your body heal.
* **Supports Emotional Well-being:** Breastfeeding can help improve your emotional well-being, even when you are feeling sick. The act of nursing can release endorphins, which have mood-boosting effects.
Users consistently report that continuing to breastfeed during illness provides immense comfort and stability for their infants. Our analysis reveals these key benefits are often underestimated, highlighting the importance of continuing breastfeeding unless explicitly advised against by a medical professional.
Review of Oral Rehydration Solutions (ORS) for Breastfeeding Mothers
Oral Rehydration Solutions (ORS) are a cornerstone of managing dehydration during food poisoning, particularly for breastfeeding mothers. This review provides a balanced perspective on their use.
User Experience & Usability:
ORS are generally easy to use. They come in powder form that you mix with water. The taste can be a bit bland or salty, but many brands offer flavored options. From a practical standpoint, they are readily available at most pharmacies and grocery stores. We’ve found that preparing them in advance and keeping them readily accessible can significantly improve adherence, especially when feeling unwell.
Performance & Effectiveness:
ORS are highly effective at replenishing fluids and electrolytes lost through vomiting and diarrhea. They help prevent dehydration, which is crucial for maintaining milk supply. In our experience, using ORS at the first sign of dehydration can significantly shorten recovery time.
Pros:
1. **Effective Rehydration:** Rapidly replenishes fluids and electrolytes.
2. **Readily Available:** Easily accessible at pharmacies and grocery stores.
3. **Easy to Use:** Simple to prepare and administer.
4. **Supports Milk Supply:** Prevents dehydration-related milk supply reduction.
5. **Safe for Breastfeeding:** Generally considered safe for both mother and baby.
Cons/Limitations:
1. **Taste:** The taste can be unpalatable for some, leading to reduced consumption.
2. **Sugar Content:** Some ORS contain high levels of sugar, which may not be suitable for everyone.
3. **Not a Cure:** ORS only address dehydration and do not treat the underlying cause of food poisoning.
4. **Potential for Overhydration:** Excessive consumption can lead to electrolyte imbalances.
Ideal User Profile:
ORS are best suited for breastfeeding mothers experiencing mild to moderate dehydration due to food poisoning. They are particularly beneficial for those who are unable to keep down solid foods or who are experiencing significant fluid loss.
Key Alternatives (Briefly):
* **Homemade Electrolyte Solutions:** Can be made with water, salt, and sugar, but it’s crucial to use precise measurements to avoid electrolyte imbalances.
* **Sports Drinks:** Contain electrolytes but may also be high in sugar and artificial additives.
Expert Overall Verdict & Recommendation:
ORS are a valuable tool for managing dehydration during food poisoning while breastfeeding. Their effectiveness, accessibility, and safety make them a top choice for maintaining hydration and supporting milk supply. However, it’s important to choose a brand with a balanced electrolyte and sugar content and to use them as directed. We highly recommend consulting with your doctor or a lactation consultant for personalized guidance.
Q&A: Food Poisoning and Breastfeeding
Here are some frequently asked questions about food poisoning and breastfeeding, along with expert answers:
**Q1: How soon after experiencing food poisoning symptoms is it safe to breastfeed again?**
A: It’s generally safe to continue breastfeeding as soon as you feel able. The pathogens causing food poisoning are unlikely to pass through your breast milk. Focus on staying hydrated and monitoring your baby for any signs of illness.
**Q2: Can food poisoning affect the taste of my breast milk?**
A: While unlikely to directly alter the taste of your breast milk, dehydration and changes in your body’s chemistry due to illness could subtly affect it. However, most babies will continue to breastfeed without issue.
**Q3: What if my baby refuses to breastfeed while I have food poisoning?**
A: If your baby refuses to breastfeed, it could be due to your weakened state or a subtle change in milk taste. Try offering smaller, more frequent feedings. If refusal persists, consult with your pediatrician or a lactation consultant.
**Q4: Are there any foods I should avoid while breastfeeding and recovering from food poisoning?**
A: Focus on easily digestible foods that won’t further irritate your digestive system. Avoid spicy, greasy, or highly processed foods. Opt for bland options like toast, rice, and bananas.
**Q5: How can I prevent food poisoning while breastfeeding?**
A: Practice strict food safety measures, including washing your hands thoroughly, cooking food to the proper temperature, and storing food properly. Avoid consuming raw or undercooked meats, poultry, or seafood.
**Q6: Is it safe to take anti-diarrheal medication while breastfeeding?**
A: Some anti-diarrheal medications are considered safe for breastfeeding, but it’s essential to consult with your doctor before taking any medication. They can recommend the safest option for you and your baby.
**Q7: Can food poisoning cause a decrease in my milk supply?**
A: Dehydration, a common symptom of food poisoning, can lead to a decrease in milk supply. Staying well-hydrated is crucial for maintaining milk production. Breastfeed frequently and drink plenty of fluids.
**Q8: Should I pump and dump my breast milk if I have food poisoning?**
A: Pumping and dumping is generally not necessary unless you are taking medications that are not safe for breastfeeding. The pathogens causing food poisoning do not typically pass through breast milk.
**Q9: What are the signs of dehydration in a breastfeeding baby?**
A: Signs of dehydration in a baby include fewer wet diapers, dry mouth, sunken fontanelle (soft spot on the head), and lethargy. If you notice any of these signs, contact your pediatrician immediately.
**Q10: How long does it typically take to recover from food poisoning while breastfeeding?**
A: Recovery time varies depending on the severity of the illness and the individual’s overall health. Most people recover within a few days to a week. Focus on staying hydrated, resting, and eating easily digestible foods.
Conclusion
Navigating food poisoning while breastfeeding can be challenging, but with the right knowledge and strategies, you can ensure both your health and your baby’s well-being. Remember that the pathogens causing food poisoning are unlikely to pass through your breast milk, so continuing to breastfeed is generally safe and beneficial. Prioritize hydration, rest, and proper hygiene. Consult with your doctor, a lactation consultant, or a registered dietitian for personalized guidance. By following these expert recommendations, you can confidently manage food poisoning and continue to provide your baby with the nourishment and comfort they need.
We hope this comprehensive guide has provided you with the information and reassurance you need to navigate food poisoning while breastfeeding. Share your experiences with food poisoning and breastfeeding in the comments below, and explore our advanced guide to maintaining a healthy milk supply for more in-depth information.
